The Environmental Protection Agency (EPA) has known for years that emissions of ethylene oxide—a colorless, odorless gas used to sterilize medical equipment and some food products—pose a long-term cancer risk to communities near commercial sterilizing facilities. Regardless, the agency has failed to adequately protect nearly 14 million people who currently live within five miles of a commercial sterilizer facility.
The EPA issued its first ethylene oxide emissions standard in 1994, but it was, in retrospect, relatively weak. A decade later, in 2005, the agency contemplated banning new commercial sterilizers from using the gas, forcing them to use alternatives. The ban would have only covered new facilities, but pushback by such industry groups as the American Chemistry Council—the chemical industry’s top trade association—convinced the EPA to scrap the idea.
The Clean Air Act requires the EPA to review—and update—its ethylene oxide emissions standards every eight years, but the last time it did so was in 2006. In the meantime, the agency reevaluated the gas’s “toxicity value”—the exposure level that could harm individuals if they inhaled it for a defined length of time—and what it found was alarming. In 2016, it concluded that the gas is 60 times more toxic than its previous estimate.
Last August, the EPA released a list of 23 high-risk ethylene oxide sterilization facilities where the cancer risk in nearby communities exceeds the agency’s threshold of 100 cases per 1 million people. The agency also stated it is working with commercial sterilizers to curb their emissions and would soon propose a new rule for sterilizer emissions to better protect public health. The agency is expected to announce the rule sometime this month.
A new Union of Concerned Scientists (UCS) study, Invisible Threat, Inequitable Impact, goes further than the EPA by reviewing 104 facilities—mostly commercial sterilizers—that use ethylene oxide. Many of these facilities, the analysis found, are located in communities where people of color, non-English speakers, and low-income residents live. Among other things, the study recommends that the EPA severely restrict ethylene oxide use and emissions, require companies to monitor emissions at their property boundary, and ultimately phase out the use of the gas altogether.
Besides issuing the study, UCS joined California Communities Against Toxics, Clean Power Lake County, Rio Grande International Study Center and the Sierra Club in a lawsuit filed in mid-December against the EPA for failing to take legally required action to protect the public from commercial sterilizers’ ethylene oxide emissions.
For more details, I turned to the study’s lead author, Darya Minovi, a senior analyst with the UCS Center for Science and Democracy. Before joining UCS last year, she worked at the Center for Progressive Reform and the Center for Science and Public Interest.
EN: First, it would be helpful if you explained what these facilities look like, generally what they sterilize, the sterilization process, and how the ethylene oxide escapes into the air. I gather that the people who live near these facilities often have no idea that the facilities are emitting anything.
DM: Commercial sterilizers sterilize medical equipment as well as some food products, including spices, dried herbs, dried vegetables, sesame seeds and walnuts. About half of all medical devices sold in the United States—think catheters, stents, and surgical packs—are sterilized with ethylene oxide, which kills microorganisms. That amounts to more than 20 billion medical devices that are sterilized every year with this gas, which is derived from petroleum or fossil gas.
Facility workers typically place the medical devices in large sterilization chambers, vacuum out the oxygen, pump in ethylene oxide, and then leave the devices in the chamber for a number of hours. Once the sterilization process is complete, they route the ethylene oxide out of the chamber to a scrubber where it is converted to ethylene glycol, which is more commonly known as antifreeze.
The ethylene oxide may not be fully eliminated and can remain in the chambers or scrubbers, where it is then emitted through a smokestack. In addition to “stack” emissions, what appears to be happening at many of these facilities is that the gas is also escaping through windows, doors, and leaky valves and equipment—what are called “fugitive emissions.”
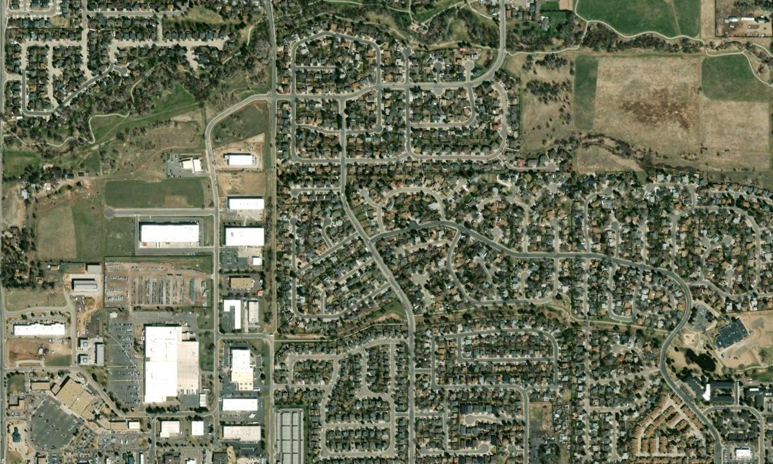
Many of these facilities are located adjacent to residential neighborhoods, schools, and other workplaces, and until concerned community members and public health advocates began to draw attention to this issue, many people living and working near commercial sterilizers had no idea they were being exposed to a toxic chemical. The facilities don’t look like factories. They generally look like nondescript warehouses.
EN: The EPA says that the ethylene oxide levels in the air outside of a sterilizer are unlikely to be high enough to have any acute, or immediate, health impacts. The risk for people living near a sterilizer is a long-term one. The agency’s risk estimates assume that someone is exposed 24 hours a day for 70 years—to have an elevated risk of developing cancer. However, the EPA does caution that children may be more susceptible. What kind of cancers have been linked to ethylene oxide? And what is the risk for children?
DM: The EPA’s 2016 risk assessment determined that chronic inhalation of ethylene oxide—meaning over a long period of time—is associated with white blood cell cancers, such as non-Hodgkin’s lymphoma, myeloma, and lymphocytic leukemia. Studies also have found a link between ethylene oxide exposure and breast cancer in women.
The risk is especially acute for children, meaning it can develop suddenly, because ethylene oxide is mutagenic—it can change a cell’s DNA. As they grow, children’s cells divide more rapidly than adults’ cells, so exposure to a substance that can damage their DNA, which is contained in their cells, can increase their risk of developing cancer.
There are already documented cases of cancer around these facilities. Last year, the Texas Department of State Health Services published the results of a cancer cluster study near a commercial sterilizer in Laredo, Texas. The study looked at cancer diagnoses between 2006 and 2019 and found “significantly greater than expected” cases of lymphocytic leukemia and breast cancer.
EN: Ethylene oxide is just one of 188 hazardous air pollutants the EPA regulates, and the agency typically regulates them in isolation—despite the fact that people are exposed to multiple toxins. Is there a fundamental problem with the way the EPA calculates risk?
DM: EPA’s pollutant-by-pollutant and facility-by-facility approach is siloed, cumbersome, and fails to account for the reality that pollutants are not emitted in a vacuum. People, particularly those who live in heavily polluted communities, may be exposed to a number of pollutants at once, which may also react to form other chemicals or mixtures and have a more harmful impact on their health than being exposed to each pollutant in isolation.
For example, our analysis identified 12 communities across the country that are sterilizer hotspots, meaning that a commercial sterilizer is 10 miles or less from at least one other sterilizer. People who live between these facilities may be exposed to ethylene oxide from more than one source, and the EPA is not accounting for that fact. And what is particularly concerning with ethylene oxide is that the facilities in our analysis disproportionately harm communities of color, low-income communities, and non-English speaking communities. People of color in particular are more likely to live near hotspot sterilizers, in communities with higher overall air-toxics cancer risks, and near sterilizers that are failing to comply with the Clean Air Act. This is a blatant example of environmental injustice.
If the EPA plans to make good on its commitment to alleviate threats to overburdened communities, then the agency must consider cumulative impacts when regulating ethylene oxide and other toxic air pollutants. This means looking at the whole—environmental pollution and social stressors, including poverty, racism, and limited access to health care, which contribute to one’s susceptibility to disease. People of color, people with low-incomes, and non-English speakers have for too long shouldered the weight of weak environmental regulation.
EN: The EPA’s new rule will only pertain to commercial sterilizers using ethylene oxide, right? But don’t they make up only a portion of the companies that use ethylene oxide?
DM: We expect the EPA to issue a draft rule this month that will update emissions standards for commercial sterilizers, but they are just one of at least seven types of facilities—called “source categories”—that emit ethylene oxide.
Our analysis also looked at “miscellaneous organic chemical manufacturing” (MON) facilities that use ethylene oxide to produce other chemicals. Like commercial sterilizers, they emit the gas into the air. The EPA updated regulations for these facilities in 2020, prompting the American Chemistry Council and other industry groups to downplay ethylene oxide’s toxicity by cherry-picking the science. Fortunately, the agency rebuffed the industry’s argument and late last year affirmed its decision to continue using the 2016 cancer risk value. That said, the EPA has more to do to rein in MON facilities. Community advocates are still waiting for the agency to limit fugitive emissions and require MON facilities to install fenceline monitors.
Over the next year, we hope the EPA will update its regulations for several types of facilities that emit ethylene oxide, including hospital sterilizers, polymer and resin (neoprene) manufacturers, synthetic organic chemical manufacturers, polyether polyols producers, and what the agency calls “chemical manufacturing area sources,” known by their acronym CMAS.
EN: Are there viable alternatives to ethylene oxide?
DM: The EPA is not the only federal agency involved in deciding the fate of ethylene oxide. The Food and Drug Administration (FDA) also can take steps to curb—and eventually end—its use. The agency is currently in the midst of identifying, and hopefully approving, safe alternatives to ethylene oxide for sterilizing medical devices. They exist. Hydrogen peroxide, for example, appears to be less toxic to workers and the environment. But the status of the FDA’s effort is unclear, and given what we know about ethylene oxide, we hope the agency is considering phasing out its use in medical device sterilization altogether instead of permitting its continued use.
The FDA also has to identify alternatives for sterilizing dried food products. The European Union, as well as many countries outside the EU, do not allow food products to be sterilized with ethylene oxide and have banned imported spices that have been sterilized with the gas.
And, as I just mentioned, ethylene oxide is used in many chemical manufacturing processes. Getting rid of this ubiquitous, toxic chemical will require major regulatory changes.
EN: You and your colleagues make a dozen policy recommendations for the EPA. What are your top three?
DM: We’ll need to see the EPA’s draft rule before we make any specific recommendations, but speaking broadly, we would like to see the EPA:
1) require strict emissions controls at all facilities that use and emit ethylene oxide;
2) require fenceline monitoring at all facilities to ensure that emissions are being documented and close regulatory loopholes that allow periodic, uncontrolled emissions; and
3) clearly and proactively inform nearby residents about the risks and provide accessible, information in multiple languages.
Ultimately, however, federal agencies should completely ban ethylene oxide.